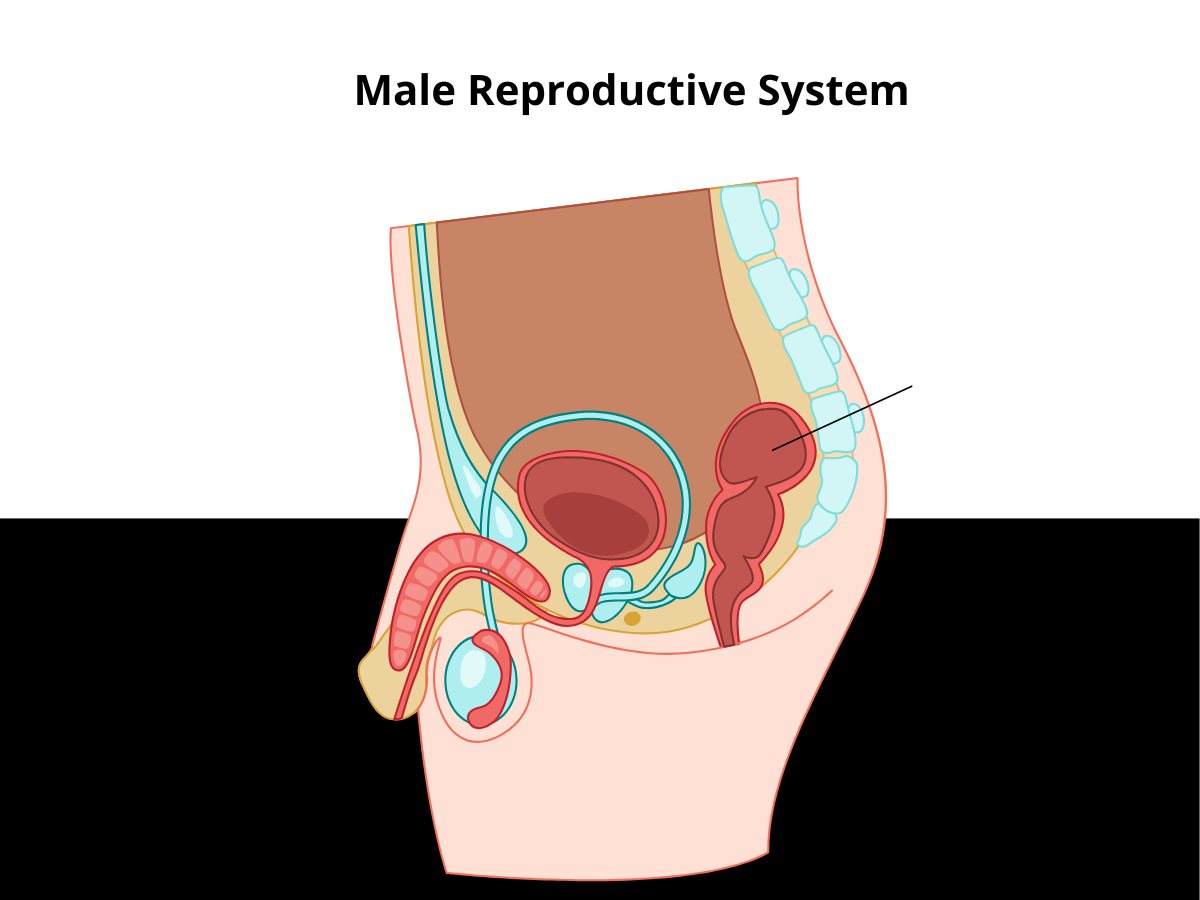
Introduction to the Male Reproductive System
The male reproductive system is a sophisticated network designed for the production, storage, and transport of sperm. Key components include the testes, epididymis, vas deferens, prostate gland, urethra, and bladder. The epididymis, a tightly coiled tube located at the back of each testicle, is essential for storing and maturing sperm before they travel through the vas deferens during ejaculation.
This system is closely linked to the urinary tract, making it susceptible to various infections. Urinary tract infections and sexually transmitted infections are among the most common causes of inflammation in the male reproductive system, including epididymitis. Because the epididymis connects directly to both the urinary tract and the vas deferens, infections can easily spread, leading to symptoms such as pain, swelling, and discomfort. Understanding how these organs work together is crucial for diagnosing and effectively treating conditions like epididymitis.
Understanding Epididymitis
Epididymitis is a common condition involving inflammation of the epididymis—the coiled tube located behind each testicle that stores and transports sperm. Epididymitis is characterized by an inflammatory process affecting the epididymis, which leads to pain and swelling.
It’s one of the leading causes of testicular pain in men under 50, yet it often goes undiagnosed or misdiagnosed.
According to a 2023 study published in the Journal of Urology, approximately 600,000 cases of epididymitis are reported annually in the U.S. Early detection and treatment are key to avoiding complications like epididymo-orchitis, infertility, and chronic pelvic pain.
Epididymitis Symptoms
Recognizing the symptoms early helps prevent progression and complications. Common signs include:
- Pain in the scrotum
- One-sided scrotal pain or swelling
- Redness or warmth in the scrotum
- Painful urination or frequent urge to urinate
- Penile discharge (white, yellow, or green)
- Fever and chills (in acute cases)
- Discomfort during intercourse or ejaculation
- Fluid buildup around the testicle (hydrocele)
In some cases, pain may radiate to the lower abdomen, which can help differentiate between various acute scrotal conditions.
In chronic epididymitis, symptoms may persist for over six weeks, usually as dull, aching pain in the testicle or groin.
⚠️ Testicular torsion may mimic epididymitis but is a medical emergency. Immediate evaluation is essential for sudden, severe testicle pain.
Types of Epididymitis
Acute Epididymitis
- Lasts < 6 weeks
- Often caused by bacterial infections, including those caused by sexually transmitted pathogens such as Chlamydia trachomatis and gonococcal infection (Neisseria gonorrhoeae), or by urinary tract infections (UTIs)
- May present with fever, scrotal tenderness, and swelling
Presumptive treatment is often initiated based on the most likely causative organisms before laboratory confirmation.
Chronic Epididymitis
- Lasts >6 weeks
- May result from prior infections, trauma, or autoimmune reactions
- Symptoms are less intense but persistent
📌 A 2024 study in European Urology Open Science found that chronic cases respond better to anti-inflammatories, pelvic floor therapy, and lifestyle adjustments than antibiotics alone.
Causes and Risk Factors
Common Causes of Epididymitis
Understanding the underlying causes of epididymitis is key to preventing recurrence and tailoring effective treatment. While the causes can vary by age, lifestyle, and health history, here are the most common culprits:
1. Sexually Transmitted Infections (STIs)
In sexually active men under 35, Chlamydia trachomatis and Neisseria gonorrhoeae are the most frequent infectious agents. These bacteria ascend through the urethra, prostate, and vas deferens to infect the epididymis.
- Often linked to unprotected sex or multiple sexual partners.
- STIs may be asymptomatic, so routine screening is essential.
2. Urinary Tract Infections (UTIs)
Escherichia coli (E. coli) and other non-sexually transmitted bacteria can cause epididymitis, particularly in older men or those with urinary tract problems.
- These bacteria can migrate from the bladder or urethra, especially when urination is obstructed or incomplete.
3. Tuberculosis (TB)
Though rare, tuberculous epididymitis can occur when Mycobacterium tuberculosis spreads from another site of infection (commonly the lungs).
- Often seen in individuals with weakened immune systems or from TB-endemic areas.
- Can cause chronic inflammation and granuloma formation in the epididymis.
4. Epididymo-Orchitis
In more severe infections, the inflammation can spread from the epididymis to the testicle, a condition known as epididymo-orchitis.
- Often presents with more intense scrotal pain, swelling, and fever.
- Can lead to testicular damage or infertility if untreated.
5. Chemical Epididymitis
This non-infectious form occurs when urine flows backward into the epididymis, often due to heavy lifting, straining, or trauma.
- Associated with conditions like reflux of sterile urine from the bladder into the vas deferens.
Risk Factors of Epididymitis
Several factors can increase a man’s risk of developing epididymitis. Awareness and prevention can significantly reduce the chances of infection or recurrence.
1. Unprotected Sex or Multiple Partners
- Engaging in unprotected sexual activity increases exposure to STIs like chlamydia and gonorrhea, which are leading causes of epididymitis in younger men.
- Regular STI screening and condom use significantly reduce this risk.
2. Use of Urinary Catheters or Medical Devices
- Indwelling catheters or intermittent self-catheterization can introduce bacteria into the urinary tract, especially in hospitalized or elderly patients.
- Any foreign object in the urinary system increases infection risk.
3. Recent Pelvic or Urological Surgery
- Procedures such as prostate surgery, vasectomy, or cystoscopy may disrupt normal urinary flow or introduce pathogens.
- Post-operative inflammation can also mimic or trigger epididymitis.
4. Urinary Tract Structural Abnormalities
- Conditions like urethral strictures, prostatic hypertrophy, or congenital malformations may impair urine flow and increase the chance of retrograde bacterial ascent.
- Chronic retention or incomplete bladder emptying compounds the risk.
5. Use of Certain Medications (e.g., Amiodarone)
- The antiarrhythmic drug amiodarone has been associated with a rare side effect of chemical epididymitis, especially at doses >200 mg/day.
- Typically non-infectious and resolves upon discontinuation.
6. History of Prostatitis or Tuberculosis
- Chronic or recurrent prostatitis (inflammation of the prostate) can serve as a reservoir for bacteria that spread to the epididymis.
- Past or latent tuberculosis infections should raise suspicion in persistent or unusual cases.
7. High-Impact Physical Activities
- Activities like long-distance cycling, heavy lifting, or motorcycling can irritate or traumatize the perineal and scrotal area, leading to inflammation or increased susceptibility to infection.
- Wearing protective gear and taking regular breaks can help reduce the risk.
Diagnosing Epididymitis: How Is It Identified
Physical Examination
Your doctor may assess:
- Swelling, tenderness, or lumps in the scrotum
- Penile discharge
- Enlarged or tender prostate (via rectal exam)
Diagnostic Tests
- Urinalysis and urine culture: To identify bacterial causes
- STI screening: To test for chlamydia or gonorrhea
- Scrotal ultrasound: To distinguish epididymitis from testicular torsion or tumors
- Blood tests: To assess for infection or inflammation
Differential Diagnosis: Ruling Out Other Conditions
Diagnosing epididymitis requires careful consideration, as its symptoms can overlap with several other serious conditions. One of the most critical distinctions is between epididymitis and testicular torsion—a surgical emergency that can threaten testicular viability if not treated promptly. Both conditions can present with acute scrotal pain, but testicular torsion typically involves sudden, severe pain and requires immediate intervention.
Other conditions that may mimic the symptoms of epididymitis include orchitis (inflammation of the testicle), testicular cancer, testicular infarction (loss of blood supply to the testicle), and mumps orchitis, especially in younger males. A thorough medical history, including recent sexual activity, number of sexual partners, and any previous urinary tract infections, helps identify risk factors and guide the diagnostic process.
A comprehensive physical examination is essential, often followed by diagnostic tests such as urinalysis, urine culture, and scrotal ultrasound. These steps help rule out other causes of scrotal pain and confirm the diagnosis of epididymitis. Considering all possible differential diagnoses ensures that patients receive the correct treatment and avoid complications from missed or delayed diagnoses.
Epididymitis Diagnosed: What to Expect Next
Once epididymitis is diagnosed, the primary goal is to treat the underlying bacterial infection and manage symptoms. Most patients will begin a course of antibiotic treatment tailored to the specific bacteria identified, which is crucial for resolving the infection and preventing complications. In addition to antibiotics, doctors often recommend supportive measures to relieve discomfort, such as resting, applying ice packs to the scrotum, and elevating the scrotum to reduce swelling.
For those experiencing severe pain, pain medications or anti-inflammatory drugs may be prescribed. It’s important to complete the entire course of antibiotics, even if symptoms improve, to ensure the infection is fully eradicated. Patients should also monitor for signs of complications, such as epididymo-orchitis, and seek medical attention if symptoms worsen or fail to improve. Regular follow-up appointments help ensure that the infection has cleared and that no further treatment is needed.
Bacterial Epididymitis: Treating the Root Cause
When caused by bacteria, especially in younger men, prompt antibiotic treatment is essential to prevent progression to severe infection and to support overall disease control. Supportive measures such as scrotal elevation, cold packs, and activity limitation are also recommended to reduce pain and swelling.
Standard Treatment Includes:
- Antibiotics: Ciprofloxacin, doxycycline, or ceftriaxone depending on the pathogen
- NSAIDs: To reduce inflammation and pain
- Scrotal support: Elevation and cold packs for symptom relief
- Sexual partner treatment: To prevent reinfection if STI is confirmed
The Role of Pelvic Floor Physical Therapy
While antibiotics remain the first line of treatment, pelvic floor physical therapy has shown promise in speeding up recovery, particularly in chronic or treatment-resistant cases.
Benefits of Physical Therapy:
- Improves pelvic blood flow
- Relieves pressure and muscular tension in the groin
- Helps with urination and ejaculation-related pain
- Reduces inflammation without side effects
💡 Clinical evidence suggests pelvic floor therapy improves outcomes when combined with medication for both acute and chronic cases.

How to Maintain a Healthy Male Reproductive System
Preventing epididymitis starts with proactive care of the male reproductive and urinary systems:
- Practice safe sex and limit sexual partners
- Stay hydrated and urinate regularly
- Avoid prolonged sitting or repetitive groin trauma
- Seek care for urinary symptoms early
- Incorporate pelvic floor exercises under professional supervision
Maintaining a healthy male genitourinary tract is essential to reduce the risk of infections and inflammation that can lead to conditions like epididymitis.
Complications of Untreated Epididymitis
If not addressed, epididymitis can lead to:
- Testicular torsion
- Infertility: Due to scarring or blocked sperm flow
- Chronic pain
- Abscess formation
- Increased risk of testicular cancer (in rare cases)
Severe or untreated cases may also result in complications involving the spermatic cord, such as abscess formation or impaired blood flow.
Prognosis: What’s the Outlook?
The outlook for most men diagnosed with epididymitis is positive, especially when treatment is started early. With appropriate antibiotic therapy and supportive care, symptoms typically resolve within a few weeks. However, if left untreated, epididymitis can lead to more serious complications, including epididymo-orchitis, testicular infarction, and even infertility due to scarring or damage to the reproductive tract.
Certain individuals, such as those with chronic epididymitis or underlying conditions like human immunodeficiency virus (HIV), may be at increased risk for persistent symptoms or complications. In these cases, ongoing management and lifestyle modifications may be necessary to control symptoms and prevent recurrence. Regular follow-up with a healthcare provider is essential to monitor recovery, address any lingering issues, and reduce the risk of long-term damage to the male reproductive system. Practicing safe sex and seeking prompt medical care for urinary or reproductive symptoms are key steps in maintaining reproductive health and preventing future episodes.
When to Seek Medical Help
Seek immediate care if you experience:
- Sudden, severe testicular pain
- Fever, chills, or nausea with groin pain
- Discharge from the penis
- Swelling that doesn’t improve in 48 hours
- Difficulty urinating
Your Next Step: Expert Help Is Available
At Pelvis NYC, we specialize in helping men manage and recover from epididymitis through science-backed pelvic floor therapy. We’ve helped countless patients ease their symptoms, restore function, and prevent recurrence.

👉 Schedule your FREE 15-minute teleconsultation with one of our pelvic health experts today.
✅ Summary: Key Takeaways
- Epididymitis is inflammation of the epididymis, commonly caused by infection.
- Symptoms include scrotal pain, swelling, and urinary issues.
- Diagnosis involves exams, lab tests, and imaging.
- Early treatment with antibiotics and adjunct therapy is vital.
- Pelvic floor therapy enhances outcomes and reduces recurrence.
Related Blog: The Ultimate Guide to Chronic Epididymitis Relief—Backed by Science – Pelvis.nyc