Low back pain is a common issue that affects millions of people worldwide. Whether it’s a persistent ache from sitting too long or a sudden sharp pain after lifting something heavy, low back pain can be a significant inconvenience. Fortunately, there are numerous treatments available that can help alleviate this discomfort and improve your quality of life. In this blog, we’ll explore the most effective treatments for low back pain, focusing on various strategies for back pain relief, so you can find the relief you need.
Chronic Back Pain and How to Relieve Pain
Chronic low back pain, defined as pain lasting longer than three months, can be particularly challenging to manage. Unlike acute pain, which is often linked to a specific injury or event, chronic pain may persist even after the initial cause has healed or subsided. This persistent discomfort can significantly impact your daily life, affecting your ability to work, exercise, and enjoy activities you once loved.
Managing chronic low back pain often requires a multi-faceted approach. This might include a combination of physical therapy, lifestyle modifications, and advanced treatment options like spinal decompression therapy or injections. For many individuals, regular physical therapy sessions focusing on strengthening and flexibility exercises are key to managing chronic pain. Additionally, pain relief medications, heat and cold applications, and manual therapy techniques like massage or chiropractic care can also play a crucial role in alleviating discomfort.
When conservative treatments are not enough, exploring advanced options like spinal decompression therapy or surgical interventions may be necessary. Consulting with a healthcare professional is essential to developing a personalized treatment plan that targets the root cause of your pain and provides long-term relief. By taking a proactive approach and exploring various treatments, you can effectively manage chronic low back pain and regain control over your life.
What Causes Low Back Pain?
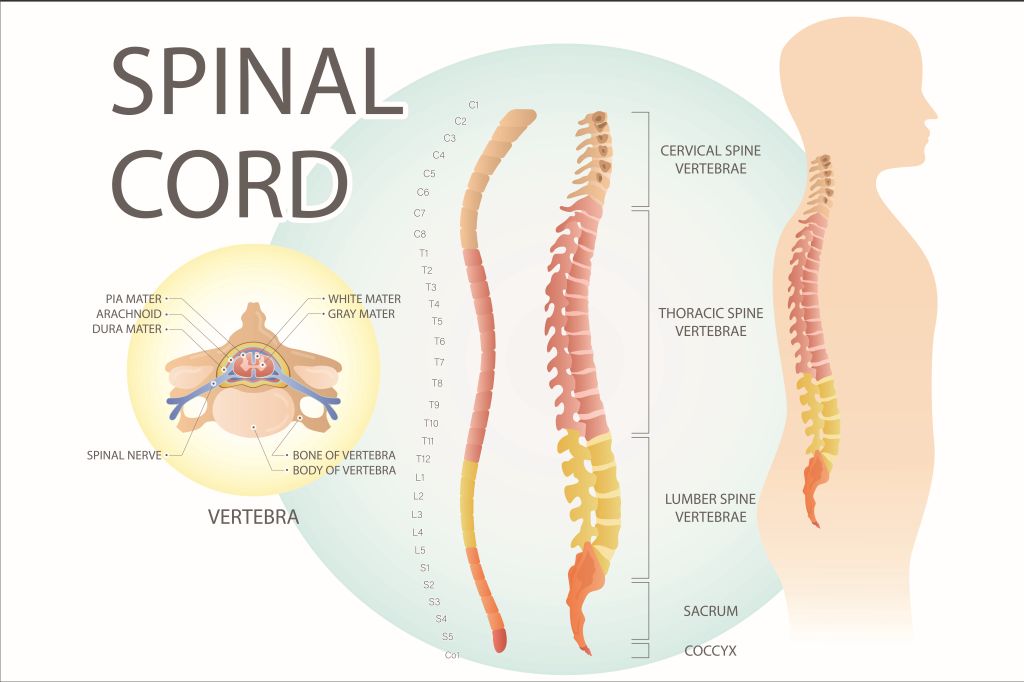
Before exploring treatment options, it’s important to understand what might be causing your low back pain. Muscle spasms can also be a cause of low back pain. The lower back, also known as the lumbar region, is a complex network of bones, muscles, ligaments, nerves, and discs that work together to support your body. Pain in this area can result from a variety of factors, such as muscle strain, poor posture, herniated discs, arthritis, or even stress. Whether the pain is acute (short-term) or chronic (lasting more than three months), addressing the root cause is key to effective treatment.

Non-Surgical Approaches for the Treatments of Low Back Pain
1. Physical Therapy
Physical therapy is often one of the first treatments recommended for low back pain. A physical therapist can develop a customized exercise plan designed to strengthen the muscles that support your back, including the abdominal muscles, improve flexibility, and enhance posture. Strengthening both back and abdominal muscles is crucial for improving posture and preventing the recurrence of pain. Exercises might include stretching, core strengthening, and low-impact aerobic activities like swimming or cycling. Physical therapy not only helps to relieve pain but also prevents future back issues.
2. Pain Relief Medications
Over-the-counter medications like ibuprofen or acetaminophen are commonly used to manage mild to moderate low back pain. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin, are particularly effective because they reduce inflammation and swelling, unlike acetaminophen which does not target inflammation. For more intense pain, a doctor may prescribe stronger medications, including muscle relaxants or anti-inflammatory drugs. Always consult a healthcare professional before starting any new medication to ensure it’s appropriate for your specific condition.
3. Heat and Cold Applications
Applying heat or cold to the painful area can offer temporary relief from low back pain. Cold packs can reduce inflammation and numb sore areas, while heat therapy can promote blood flow and relax tight muscles. Alternating between heat and cold can be especially effective for managing pain and reducing stiffness.
4. Manual Therapy Techniques
Manual therapy, such as chiropractic adjustments and massage, can also be beneficial for those suffering from low back pain. Chiropractors use hands-on methods to adjust the spine and improve its alignment, while massage therapists focus on relieving muscle tension and improving circulation. Both approaches can significantly reduce pain and enhance overall well-being.
5. Lifestyle Changes
Making certain lifestyle adjustments can play a critical role in managing low back pain. This might include improving your posture, using ergonomic furniture, maintaining a healthy weight, and incorporating regular physical activity into your daily routine. Avoiding activities that place undue strain on your back is also essential for long-term relief.
Advanced Treatments for Low Back Pain
1. Injections
When conservative treatments aren’t enough, injections may be considered. Pain affects daily activities and functional abilities, making it crucial to find effective relief options. Corticosteroid injections can help reduce inflammation around irritated nerves, providing temporary pain relief. Nerve blocks are another option, designed to interrupt pain signals and provide short-term relief. While these treatments can be effective, they are usually part of a broader pain management plan.
2. Spinal Decompression Therapy
Spinal decompression therapy is a non-invasive treatment that gently stretches the spine to relieve pressure on the discs and nerves. Maintaining the integrity of spinal bones is crucial in preventing conditions like herniated discs or spinal stenosis. This therapy is particularly beneficial for conditions like herniated discs or spinal stenosis, where reducing spinal pressure can lead to significant pain relief.
3. Surgical Interventions
Surgery is generally considered a last resort for low back pain, reserved for severe cases that don’t respond to other treatments. Surgical options may include spinal fusion, laminectomy, or discectomy, depending on the specific issue. Surgery aims to stabilize the spine or remove damaged tissues, providing relief when other treatments have failed.
When to Consult a Healthcare Professional
While many cases of low back pain can be managed with self-care and conservative treatments, there are times when professional help is necessary. Physical therapists play a crucial role in diagnosing and treating low back pain by improving flexibility, strengthening muscles, and enhancing posture. If your pain is severe, lasts longer than a few weeks, or is accompanied by symptoms like numbness, tingling, or weakness in your legs, it’s important to consult a healthcare provider. These symptoms could indicate a more serious condition that requires prompt attention.
Conclusion: Taking Charge of Your Low Back Pain
Living with low back pain doesn’t have to be a daily struggle. By exploring a combination of treatments and making key lifestyle changes, you can effectively manage your pain and enjoy a better quality of life. Whether you’re considering physical therapy, medications, or advanced treatment options, understanding what’s available is the first step toward relief.
Ready to explore effective treatments for low back pain? Visit Pelvis NYC to learn more about how our specialized services can help you find relief and get back to living pain-free.