If you have ever thought to yourself, “I can’t get rock hard anymore,” you are not alone. Many men experience this problem at some point in their lives, and the medical term for it is erectile dysfunction or ED.
In fact, most men will experience erectile issues at some point, making it a common and manageable condition.

What Is Erectile Dysfunction and Why I Can’t Get Rock Hard Anymore
Erectile dysfunction means having trouble getting or keeping a firm enough erection for sexual intercourse. It can happen occasionally, but when it becomes frequent, it is usually a sign of an underlying issue.
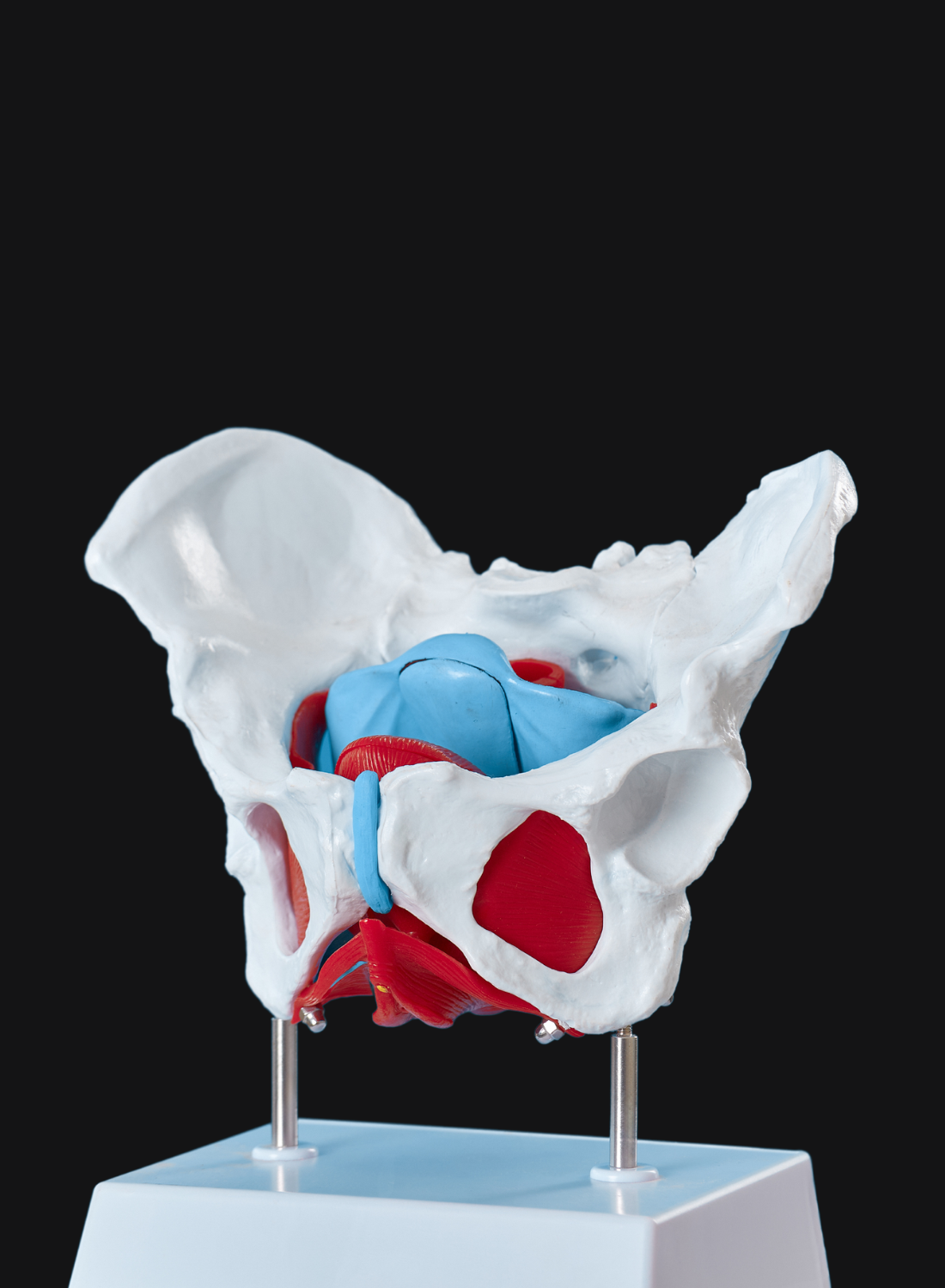
An erection depends on a smooth connection between the brain, hormones, blood vessels, nerves, and emotions. If even one part of this system is not working properly, the result can be erection problems.
Causes of Erectile Dysfunction: From Physical Causes to Psychological Treatments
Physical causes of ED
- Heart disease and cardiovascular disease problems reduce blood flow to the penis, making them major risk factors for ED.
- Abnormal blood sugar levels, as seen in diabetes, can damage blood vessels and nerves, contributing to erectile dysfunction.
- Diabetes, obesity, and high blood pressure put strain on blood vessels and are common medical conditions linked to ED.
- Physical factors such as injuries or surgeries can affect sexual function.
- Physical problems like hormonal imbalances or chronic illnesses can also lead to ED.
- Low testosterone and neurological conditions, including damage to the spinal cord or spinal cord injury, can disrupt nerve signals necessary for erections.
- Certain medications including antidepressants, blood pressure drugs, and antihistamines, may cause ED as a side effect.
- ED can be a symptom of an underlying medical condition, so identifying and addressing these medical conditions is important for effective treatment.
- Testosterone replacement may be considered for men with low testosterone levels, but it is most effective when hormone deficiency is present.
Psychological causes of ED
- Mental health conditions such as anxiety and depression can interfere with sexual function and contribute to erection problems.
- Relationship problems, including poor communication and unresolved conflicts, can negatively impact sexual performance and overall intimacy.
- Low sex drive or reduced sexual desire often accompanies erectile dysfunction, especially when psychological factors or hormonal imbalances are involved.
- Sexual problems can include both erectile dysfunction and issues like premature ejaculation, and these conditions may overlap.
- Cognitive behavioural therapy and other psychological treatments are effective in addressing these mental health factors.
Lifestyle Changes That Improve Erections and Cardiovascular Health
Healthy living makes a real difference for ED treatment. Doctors often recommend lifestyle changes before or alongside medication. Lifestyle changes are often recommended to treat erectile dysfunction, and treating erectile dysfunction may involve a combination of these strategies. These include:
- Eating a balanced diet that supports cardiovascular health
- Exercising at least 30 minutes most days of the week
- Quitting smoking and limiting alcohol
- Getting enough quality sleep
- Reducing stress through mindfulness, meditation, or therapy
These steps improve circulation, lower blood pressure, and enhance energy levels which all support stronger erections.
How Certain Medications and Treatments Can Help You Get Hard Again
When lifestyle changes are not enough, medical support is available.
- Oral ED treatments like Viagra, Cialis, Levitra, or Stendra improve blood flow and make it easier to get an erection with sexual stimulation
- Other medications may be used to manage ED, especially when first-line treatments are not suitable or effective, and should be considered with attention to possible interactions and safety.
- Vacuum erection devices and penile injections provide alternatives when pills are not effective
- Penile implant is a permanent surgical option for men who have not responded to other therapies; it involves placing a device inside the penis to allow for an erection.
- Other treatments such as psychological therapies, including cognitive behavioural therapy, sex therapy, or psychosexual counselling, can help address underlying psychological or emotional issues contributing to ED.
- Sex therapy is a psychological treatment option that can help men and couples address relationship or emotional factors affecting erectile function, often involving techniques like sensate focus and support from qualified therapists.
When to Seek Medical Advice for Erectile Dysfunction
Erectile dysfunction can feel frustrating and even distressing, but you do not have to face it alone. Occasional erection problems happen to many men, but persistent difficulty getting or maintaining an erection means it is time to seek medical advice. A healthcare professional can identify the underlying causes of erectile dysfunction and guide you to the most effective treatment options. Interested in reading – Are Guys Embarrassed When They Can’t Get It Up?
Reach out to a doctor if you suddenly develop erectile dysfunction or if ongoing erection problems disrupt your sex life or relationship. Erectile dysfunction often signals a more serious health condition such as high blood pressure, heart disease, diabetes, kidney disease, or multiple sclerosis. When you address these health problems early, you improve your sexual performance and protect your overall health.
Talk to your healthcare provider if you take certain medications such as beta blockers or other blood pressure drugs, or if you use recreational drugs. These substances affect blood flow and sexual function, and your doctor can help you weigh the risks and explore safer alternatives.
During your visit, your doctor will review your medical history, ask about your sexual activity, and evaluate both physical and psychological factors that contribute to erectile dysfunction. They may recommend erectile dysfunction medications or suggest psychological treatments like cognitive behavioural therapy if emotional issues play a role. In many cases, you can improve blood flow, strengthen cardiovascular health, and enhance your erections by making lifestyle changes such as eating a balanced diet, exercising regularly, and maintaining a healthy weight.
Erectile dysfunction is common and has many possible causes. By seeking medical advice, you take a proactive step toward improving your sexual health, building confidence, and enjoying a more satisfying sex life. Do not wait to reach out. Help is available, and effective treatments can restore your performance and quality of life.
Frequently Asked Questions About Erectile Dysfunction
Can erectile dysfunction be cured naturally?
For some men ED improves naturally through lifestyle changes such as better diet, exercise, and stress reduction. The outcome depends on the underlying cause.
At what age do erection problems usually start
Erectile dysfunction can affect men at any age but it becomes more common after age forty. Research shows that about half of men over fifty experience some degree of ED.
Is heart disease linked to erectile dysfunction?
Yes. Heart disease and other cardiovascular health problems reduce blood flow to the penis which often leads to ED. In fact, erectile dysfunction can be an early warning sign of hidden heart issues.
Can anxiety or stress cause ED?
Absolutely. Mental stress triggers adrenaline which restricts blood flow and prevents an erection. Psychological treatments such as therapy or counselling can be very effective.
What is the best ED treatment available?
The best treatment depends on the cause of erectile dysfunction. Many men respond well to oral medication. Others find that lifestyle changes, therapy, or a combination of treatments is most effective.
Key Takeaway
Thinking “I can’t get rock hard anymore” can feel discouraging, but it does not mean the end of your sex life. Erectile dysfunction is common; it is not your fault, and most importantly it can be treated. By making lifestyle changes, understanding the causes of erectile dysfunction, and exploring the right ED treatments, you can restore confidence and enjoy intimacy again.
Take the Next Step
If you are ready to address erectile dysfunction and take control of your sexual health, the team at Pelvis NYC is here to help. Our specialists focus on personalised care for men dealing with erection problems, cardiovascular health issues, and related conditions.