Experiencing pain or discomfort during urination, medically termed dysuria, can be a distressing and inconvenient issue. It’s essential to understand the causes behind this discomfort and explore potential solutions to alleviate it. In this comprehensive guide, we delve into the reasons why it hurts when you pee and discuss how physical therapy can offer relief.
Causes of Painful Urination: Urinary Tract Infection and More
There are several potential causes of painful urination, also known as urination pain:
- Urinary Tract Infection (UTI): UTIs are among the most prevalent reasons for painful urination. They occur when bacteria enter the urinary tract and multiply, leading to irritation and inflammation of the bladder and urethra. This irritation can cause discomfort or a burning sensation during urination. UTIs, often resulting from a bacterial infection, can also cause abdominal pain, indicating a possible progression to a kidney infection if left untreated.
- Urethritis: Urethritis, characterized by inflammation of the urethra, often results from bacterial infections or irritation. Bacteria from sexually transmitted infections (STIs) like gonorrhea or chlamydia, and even bacterial overgrowth, can cause urethritis, leading to pain and discomfort while urinating.
- Bladder Inflammation: Infections or other conditions that inflame the bladder, such as cystitis, can cause painful urination. This inflammation irritates the bladder lining, resulting in discomfort or pain during urination. Conditions like interstitial cystitis and painful bladder syndrome are also known to cause similar symptoms.
- Sexually Transmitted Infections (STIs): Certain STIs can lead to urethritis, causing painful urination. STIs like gonorrhea, chlamydia, and genital herpes can infect the urethra, leading to inflammation and discomfort during urination.
- Chemical Irritation: Exposure to certain chemicals or irritants can irritate the urethra and bladder, causing discomfort or pain during urination. This can occur due to contact with substances like harsh soaps, perfumes, or spermicides.
- Dehydration: When the body lacks sufficient fluids, urine becomes more concentrated. This concentrated urine can irritate the lining of the bladder and urethra, leading to discomfort or pain during urination. Additionally, dehydration can reduce the body’s ability to flush out bacteria and toxins, increasing the risk of urinary tract infections (UTIs) and further exacerbating symptoms of dysuria. Therefore, maintaining adequate hydration levels is crucial for preventing urinary discomfort and promoting overall urinary health.
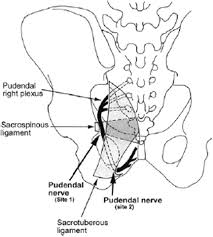
- Prostate problems: The prostate gland, surrounding the top of the urethra, plays a crucial role in urination. Issues with the prostate, such as prostatitis, may experience painful urination due to inflammation of the prostate gland.
- Kidney Infection and Kidney Stones: Kidney infections, technically called pyelonephritis, and kidney stones are significant causes of painful urination. These conditions can lead to severe abdominal pain and require immediate medical attention.
Take note that when you experience a burning sensation upon urination, it is best to see a doctor to help you find the cause of your discomfort and help with the treatment. You can also find a physical therapist who can provide you with exercises that will help achieve proper engagement of the pelvic floor muscles that regulate urine release.
Physical Therapy’s Role in Painful Urination
To treat painful urination, physical therapy emerges as a pivotal approach, addressing the discomfort associated with this condition. Physical therapists leverage targeted exercises and techniques to tackle the underlying causes, such as infections or irritants, that contribute to dysuria. They emphasize strengthening pelvic floor muscles, essential for bladder control and urinary function. By enhancing muscle tone and coordination, physical therapy can improve bladder control and relieve pressure on the urinary tract. Moreover, physical therapists may introduce relaxation techniques to diminish muscle tension and discomfort, significantly boosting urinary health and life quality for those suffering from dysuria.
How Does Physical Therapy Work?
Physical therapy for painful urination involves various techniques aimed at strengthening and relaxing specific muscles involved in bladder function. These techniques include:
- Pelvic Floor Exercises: Physical therapists often prescribe targeted pelvic floor exercises to strengthen the muscles that support the bladder, urethra, and surrounding pelvic organs. These exercises, such as Kegels, help improve muscle tone and control, reducing symptoms of dysuria and enhancing bladder function.
- Biofeedback Therapy: Biofeedback therapy involves using specialized equipment to monitor and provide feedback on muscle activity in real time. During sessions, patients learn to control and strengthen pelvic floor muscles by observing their muscle contractions on a screen. Biofeedback helps individuals develop better awareness and control over their pelvic muscles, leading to improved bladder function and reduced urinary discomfort.
- Manual Therapy Techniques: Physical therapists may employ manual therapy techniques to address muscle tension and dysfunction in the pelvic region. This may include gentle manipulation or massage of soft tissues to release tension, improve blood flow, and enhance mobility. Manual therapy can help alleviate pelvic floor muscle spasms and reduce pain associated with dysuria, promoting overall urinary function.
Choosing the Right Physiotherapist for Your Painful Urination Due to Interstitial Cystitis
We know how hard it is to find a partner who will stay with you until you say “I am FREE from PAIN NOW” especially if you are a man. However, you don’t have to be anxious because we are here to help you live a pain-free life.
At Pelvis NYC, we are dedicated to helping men ease their symptoms and improve the quality of their lives. Our physiotherapist Dr. Adam Gvili uses a variety of techniques to relieve pain, including massage, heat and cold therapies, electrical stimulation, and exercises. His treatment is specifically tailored per individual to target the right cause of the pain and employ the right treatment.
For further inquiries, visit Pelvis NYC and get a FREE 15-minute teleconsultation. Book a schedule now and let’s find the right combination of treatments to ease your pain and get you back to feeling normal again.
Related Blog: Managing Urinary Issues: Expert Tips from a Physical Therapist